AI ROI for Medical Practices: Setting Realistic Expectations
AI promises abound, but what returns can medical practices actually expect? A realistic look at AI costs, benefits, and how to measure success.

AI ROI for Medical Practices: Setting Realistic Expectations
Every AI vendor promises transformation. Dramatic efficiency gains. Massive cost savings. Revolutionary patient experiences.
The reality is more nuanced.
AI can deliver meaningful returns for medical practices—but not magic. Understanding realistic expectations helps you make better investment decisions, implement more effectively, and measure success accurately.
Here’s an honest look at AI ROI for medical practices.
The Hype vs. Reality Gap
Let’s address the elephant in the room: AI marketing often oversells.
Common Overclaims
“Reduce administrative burden by 80%”
- Reality: 30-50% reduction in specific tasks is more common
- Total administrative burden reduction is usually 15-25%
- Some tasks don’t lend themselves to AI (yet)
“Immediate results”
- Reality: Implementation takes months
- ROI typically materializes in 6-12 months
- Learning curves affect initial productivity
“Works seamlessly with your existing systems”
- Reality: Integration varies from excellent to painful
- Your specific EHR matters enormously
- Custom work is often needed
“Set it and forget it”
- Reality: AI systems need ongoing monitoring
- Regular updates and optimization required
- Staff training is continuous
Why the Gap Exists
- Vendors show best-case scenarios
- Pilots often have more support than production
- Marketing focuses on potential, not typical results
- Every practice’s situation differs
Realistic ROI by AI Application
Let’s look at actual returns for common AI applications:
Prior Authorization Automation
Typical Investment:
- $200-500/month for automation tools
- 20-40 hours implementation time
- Ongoing staff time for oversight
Realistic Returns:
- 50-70% reduction in time per authorization
- 15-25% improvement in first-pass approval rates
- Fewer denials due to documentation issues
ROI Calculation Example:
Current state: 2 FTEs spending 50% of time on prior auth = $60,000/year
With AI: Same volume handled in 60% less time = $36,000 saved
AI cost: $4,800/year + implementation
Net savings: ~$30,000/year
Payback period: 2-3 months
Verdict: Strong ROI for practices with significant prior auth volume.
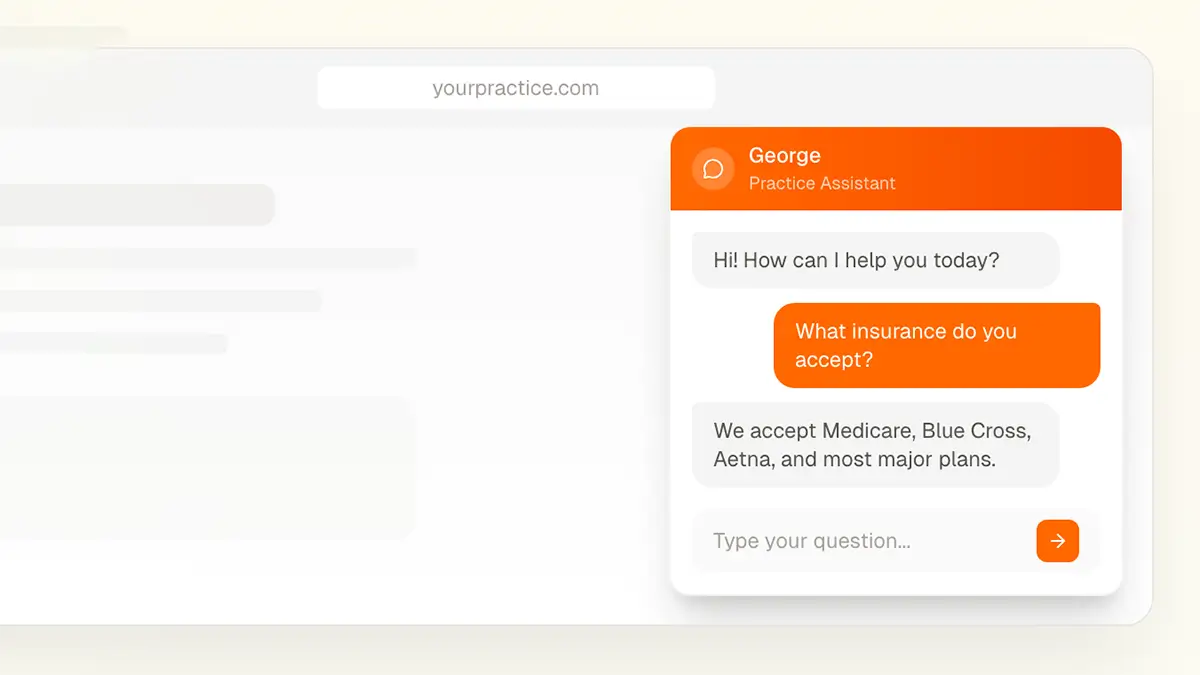
Patient Communication Chatbots
Typical Investment:
- $100-400/month for chatbot platforms
- 20-30 hours setup and content development
- Ongoing content maintenance
Realistic Returns:
- 25-40% reduction in routine phone calls
- 24/7 availability for common questions
- Improved patient satisfaction with instant answers
ROI Calculation Example:
Current state: Front desk handles 100 calls/day, 40% are routine FAQs
With chatbot: 30% of FAQ calls deflected = 12 calls/day
Time saved: 12 calls × 3 minutes = 36 minutes/day = 150 hours/year
Value: 150 hours × $25/hour = $3,750/year
Chatbot cost: $3,000/year
Net savings: $750/year plus soft benefits (after-hours coverage, satisfaction)
Verdict: Modest direct ROI; value often comes from qualitative benefits.
Digital Patient Intake
Typical Investment:
- $200-600/month for intake platforms
- 40-60 hours implementation
- Ongoing maintenance and updates
Realistic Returns:
- 80-90% reduction in data entry time
- Improved data accuracy
- Better patient experience
- Faster check-in process
ROI Calculation Example:
Current state: Staff spends 10 minutes data entry per patient, 30 patients/day = 5 hours/day
With AI intake: 90% reduction = 4.5 hours saved daily = 1,125 hours/year
Value: 1,125 hours × $22/hour = $24,750/year
Platform cost: $6,000/year + implementation
Net savings: ~$18,000/year
Verdict: Strong ROI for practices with meaningful patient volume.
Workflow Automation (General)
Typical Investment:
- $300-1,000/month depending on scope
- Significant implementation time (varies widely)
- Ongoing optimization
Realistic Returns:
- Varies enormously by specific workflows automated
- Typically 40-60% time savings on targeted tasks
- Error reduction in automated processes
Verdict: ROI depends entirely on what you automate and current inefficiency levels.
Factors That Affect Your ROI
Your results will differ based on:
Practice Size and Volume
Larger practices typically see better ROI:
- More transactions to automate
- Fixed costs spread across more patients
- More staff time available to redirect
Smaller practices may struggle with ROI:
- Lower volume means less automation benefit
- Implementation effort same regardless of size
- May not have staff time to redirect
Current Efficiency Level
Already efficient practices see smaller gains:
- Less waste to eliminate
- Existing processes may be good enough
- Incremental improvement harder to achieve
Inefficient practices see larger gains:
- More opportunity for improvement
- Bigger problems to solve
- AI impact more dramatic
Technology Foundation
Modern systems enable better ROI:
- Easier integration
- Better data quality
- More automation possibilities
Legacy systems limit ROI:
- Integration challenges
- Data quality issues
- Manual workarounds needed
Staff Capabilities
Tech-savvy teams achieve faster ROI:
- Shorter learning curves
- Better adoption
- More creative use of tools
Less tech-comfortable teams delay ROI:
- Extended training needs
- Resistance to change
- Workarounds that undermine value
Implementation Quality
Well-planned implementations maximize ROI:
- Clear goals and metrics
- Proper training
- Appropriate customization
- Ongoing optimization
Poor implementations destroy potential ROI:
- Unclear objectives
- Inadequate training
- Cookie-cutter deployment
- Set-and-forget mentality
Hidden Costs to Consider
ROI calculations often miss:
Implementation Time
Your staff’s time has value:
- Project management
- Training time
- Workflow redesign
- Testing and validation
This is real cost, even if it doesn’t show on an invoice.
Productivity Dip
New systems cause temporary slowdowns:
- Learning curve period
- Parallel processing during transition
- Error correction early on
Plan for productivity to drop before it improves.
Ongoing Maintenance
AI systems need care:
- Content updates
- Performance monitoring
- Staff retraining
- Vendor management
Budget 10-20% of implementation effort annually for maintenance.
Opportunity Cost
Resources spent on AI aren’t spent elsewhere:
- What else could that budget accomplish?
- What other projects are delayed?
- Is AI the highest-value investment?
Integration Complexity
Connecting AI to existing systems often costs more than expected:
- Custom development needs
- Data mapping and cleanup
- Testing and validation
- Ongoing integration maintenance
Measuring AI Success
Track these metrics to evaluate your AI investments:
Efficiency Metrics
Time savings:
- Hours saved per task
- Tasks completed per day
- Time-to-completion for processes
Accuracy:
- Error rates before/after
- Rework required
- Quality scores
Financial Metrics
Direct costs:
- Software/platform fees
- Implementation costs
- Ongoing maintenance
Direct savings:
- Labor cost reduction
- Error-related cost reduction
- Vendor cost changes
Revenue impact:
- Throughput changes
- Collection rate changes
- Patient retention changes
Qualitative Metrics
Staff experience:
- Satisfaction scores
- Turnover rates
- Productivity sentiment
Patient experience:
- Satisfaction scores
- Wait time perceptions
- Access and convenience feedback
Attribution Challenges
Measuring AI impact is genuinely hard:
- Multiple variables change simultaneously
- Seasonality affects comparisons
- Hawthorne effect inflates early results
- Long-term effects differ from short-term
Use before/after comparisons carefully, and acknowledge uncertainty in your ROI calculations.
Red Flags: When AI Won’t Deliver ROI
Some situations aren’t AI opportunities:
Volume too low: If you process 5 prior auths per week, automation won’t pay off.
Problem isn’t efficiency: If the issue is clinical quality or strategy, AI won’t fix it.
Foundation isn’t ready: Poor data, legacy systems, or untrained staff will undermine AI benefits.
Culture resistant: If staff won’t adopt new tools, investment is wasted.
Budget too tight: Cutting corners on implementation guarantees poor results.
Expectations unrealistic: If you expect 80% improvement and achieve 40%, you’ll be disappointed even though 40% is good.
Making Better AI Investment Decisions
Start With the Problem
Don’t buy AI because it’s exciting. Buy it because:
- You have a specific, quantifiable problem
- AI is a reasonable solution to that problem
- The expected ROI justifies the investment
Do the Math Before Buying
Calculate expected ROI based on:
- Your actual current costs (not guesses)
- Realistic improvement expectations (not vendor claims)
- Full costs including hidden costs
- Reasonable timeline to value
Start Small
Don’t bet big on unproven returns:
- Pilot before full deployment
- Start with highest-confidence use cases
- Prove ROI before expanding
Measure Honestly
Track results against predictions:
- Set baseline metrics before implementation
- Measure consistently after implementation
- Be honest about what’s working and what isn’t
Iterate Based on Data
Use results to guide future investments:
- Double down on what works
- Adjust or abandon what doesn’t
- Apply learnings to next initiative
The Bottom Line
AI can deliver meaningful ROI for medical practices—but returns vary widely based on your specific situation, the applications you choose, and how well you implement.
The practices getting the best results:
- Start with clear, quantifiable problems
- Set realistic expectations
- Implement carefully with proper support
- Measure honestly and iterate
The practices struggling with AI ROI:
- Chase technology for its own sake
- Believe vendor marketing uncritically
- Underinvest in implementation
- Fail to measure and adjust
Approach AI as a business investment requiring rigorous analysis, not a magic solution that will obviously pay off.
Need Help Evaluating AI ROI?
We help medical practices assess AI opportunities realistically and implement solutions that deliver measurable returns.
Contact us for an honest AI assessment →
Or call us directly: (678) 824-2420