AI-Powered Patient Intake: Reducing Clipboard Time and Data Entry
Digital patient intake with AI can save 15+ minutes per patient while improving data accuracy. Here's how to implement it effectively.

AI-Powered Patient Intake: Reducing Clipboard Time and Data Entry
The clipboard is healthcare’s most persistent relic.
Patients arrive, fill out the same forms they’ve filled out before, hand illegible paperwork to staff, and wait while someone types it all into the EHR. Staff spend hours on data entry. Errors creep in. Information gets lost. Everyone’s frustrated.
AI-powered digital intake doesn’t just digitize the clipboard—it transforms the entire process. Patients complete forms before arrival. AI validates and organizes the information. Staff review rather than type. And the data flows directly into your systems.
Here’s how to implement AI-powered intake that actually works.
The Problem With Traditional Intake
Let’s quantify what clipboard intake actually costs:
Time Costs
- Patient time: 15-20 minutes filling out forms in the waiting room
- Staff time: 10-15 minutes per patient entering data
- Provider time: Reviewing incomplete or unclear information during the visit
Error Costs
- Illegible handwriting causing data entry mistakes
- Transcription errors during manual entry
- Missing information discovered mid-visit
- Insurance information entered incorrectly
Experience Costs
- Patients frustrated filling out “the same forms every time”
- Waiting room backups when intake runs long
- Staff stressed by data entry burden
- Providers starting visits with incomplete information
For a practice seeing 30 patients per day, traditional intake consumes 5-8 hours of staff time daily—just on data entry.
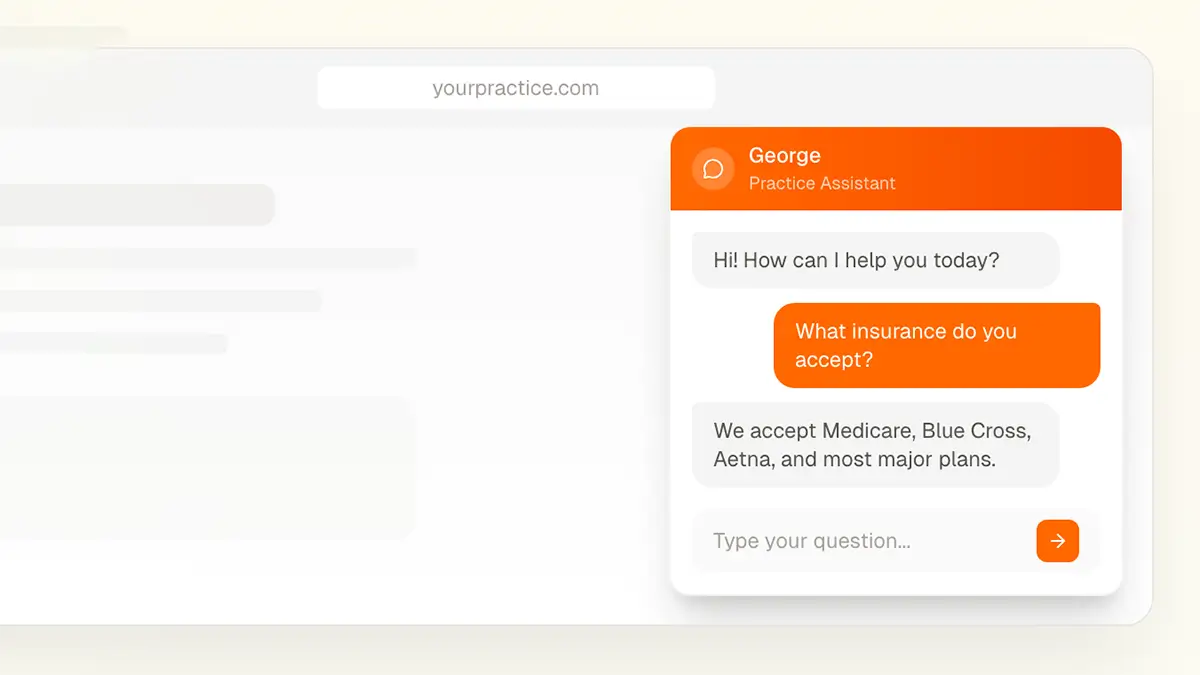
What AI-Powered Intake Looks Like
Modern intake transforms this process:
Before the Visit
Patient receives link via text or email 24-48 hours before appointment.
Patient completes forms on their phone, tablet, or computer—at home, at their convenience.
AI validates information as it’s entered:
- Flags incomplete fields
- Validates insurance information format
- Checks for logical inconsistencies
- Prompts for missing required data
Data is organized and ready for staff review before patient arrives.
At Check-In
Patient arrives with intake already complete.
Staff reviews pre-populated information rather than entering from scratch.
Updates only are needed—not full data entry.
Patient proceeds to visit faster, with complete information in the chart.
The AI Difference
What makes this “AI-powered” rather than just “digital forms”?
Intelligent validation: AI catches errors humans miss—impossible dates, invalid insurance formats, contradictory answers.
Smart follow-ups: Based on initial answers, AI asks relevant follow-up questions. Check “diabetes”? Follow-up questions about management appear.
Data extraction: AI can pull information from uploaded insurance cards, IDs, and documents.
Learning and improvement: System improves over time based on what information proves useful vs. unnecessary.
Benefits You Can Measure
Practices implementing AI intake typically see:
Time Savings
- 80-90% reduction in data entry time
- 15+ minutes saved per patient visit
- Staff redirected to higher-value activities
Accuracy Improvement
- Fewer data entry errors (no transcription)
- More complete information (required field validation)
- Better insurance accuracy (format validation)
Patient Experience
- Higher satisfaction scores (no clipboard, faster check-in)
- Reduced wait times (intake done before arrival)
- Mobile-friendly (complete on their own device)
Operational Impact
- Smoother visit flow (no intake bottlenecks)
- Fewer claim denials (accurate insurance info)
- Better prepared providers (complete information available)
Implementation Approaches
Several approaches exist for AI-powered intake:
Standalone Intake Solutions
Dedicated platforms that specialize in digital intake.
Pros:
- Purpose-built for intake
- Often best-in-class features
- Rapid implementation
Cons:
- Another system to manage
- Integration with EHR required
- Additional vendor relationship
EHR-Integrated Intake
Intake modules within your existing EHR system.
Pros:
- Native integration
- Single vendor
- Data stays in one system
Cons:
- May be less sophisticated
- Limited customization
- Dependent on EHR vendor’s priorities
Patient Portal Intake
Intake through your existing patient portal.
Pros:
- Patients already have accounts
- No new system for patients
- Integrated with portal features
Cons:
- Portal adoption may be low
- Limited AI capabilities in most portals
- May not work for new patients
Hybrid Approaches
Combining solutions for different patient types.
Example: Portal intake for established patients, standalone solution for new patients.
What to Include in Digital Intake
Not everything on your paper forms needs to be digital. Optimize for what matters.
Essential Information
Demographics:
- Name, DOB, contact information
- Emergency contact
- Preferred pharmacy
Insurance:
- Primary and secondary coverage
- Policy holder information
- Card images (front and back)
Medical History:
- Current medications
- Allergies
- Past medical history
- Surgical history
- Family history (for relevant specialties)
Visit-Specific:
- Reason for visit
- Current symptoms
- Relevant recent changes
Nice to Have
Consent forms:
- HIPAA acknowledgment
- Financial policies
- Treatment consent
Social history:
- Occupation
- Lifestyle factors relevant to specialty
Screening questionnaires:
- PHQ-9 for depression screening
- Specialty-specific assessments
Skip or Simplify
Redundant questions:
- Information you already have in the chart
- Questions that never change
Low-value questions:
- Information that doesn’t affect care
- Questions no one actually reviews
Making It Work for All Patients
Digital intake works great for tech-savvy patients. What about everyone else?
Patients Without Smartphones
- Offer tablet-based intake in office
- Allow completion on any computer
- Keep paper option available as backup
Elderly Patients
- Larger text options
- Simpler interface
- Phone support for questions
- Family member assistance allowed
Language Barriers
- Multi-language support
- Clear, simple language
- Translation assistance
Low Digital Literacy
- Intuitive interface design
- Progress indicators
- Help text throughout
- Staff assistance available
Key principle: Digital intake should be the primary path, not the only path. Some patients will always need alternatives.
Integration Considerations
For AI intake to deliver full value, it needs to connect with your systems.
EHR Integration
Ideal state: Data flows directly into correct EHR fields without manual intervention.
Reality: Integration depth varies significantly by solution and EHR. Understand exactly what “integrates with your EHR” means:
- Direct field mapping?
- PDF attachment?
- Manual review and entry still required?
Insurance Verification
Opportunity: Connect intake to real-time eligibility verification.
Benefit: Know before patient arrives whether insurance is active and what coverage exists.
Appointment Scheduling
Opportunity: Trigger intake automatically when appointments are scheduled.
Benefit: Seamless patient experience without manual link sending.
HIPAA and Compliance
Digital intake involves PHI, so compliance matters.
Vendor Requirements
- Business Associate Agreement required
- Data encryption in transit and at rest
- Access controls and audit trails
- Appropriate data retention policies
Patient Consent
- Clear explanation of how data is used
- Privacy policy acknowledgment
- Appropriate consent language
Data Security
- Secure transmission (HTTPS)
- No PHI in email subject lines
- Appropriate session timeouts
- Secure storage
Learn more about healthcare AI compliance →
Common Implementation Mistakes
Avoid these pitfalls:
Over-Complicating Forms
Mistake: Digitizing every question from your paper forms.
Result: Patients abandon lengthy forms; completion rates plummet.
Fix: Ruthlessly eliminate unnecessary questions. If no one reads the answer, don’t ask the question.
Poor Mobile Experience
Mistake: Forms designed for desktop that don’t work well on phones.
Result: Patients struggle to complete intake on their primary device.
Fix: Mobile-first design. Test on actual phones.
Inadequate Testing
Mistake: Launching without thorough testing across scenarios.
Result: Patients hit errors; staff lose confidence in system.
Fix: Test every path, every device, every edge case before launch.
Forcing Digital-Only
Mistake: Eliminating all paper options immediately.
Result: Some patients can’t complete intake; frustration all around.
Fix: Keep paper backup available, even if you don’t promote it.
Ignoring Staff Training
Mistake: Assuming staff will figure it out.
Result: Staff don’t trust the system, create workarounds, undermine adoption.
Fix: Comprehensive training before launch, ongoing support after.
Measuring Success
Track these metrics:
Adoption Metrics
- Percentage of patients completing digital intake
- Completion rate (started vs. finished)
- Time to complete
Efficiency Metrics
- Staff time spent on data entry (before/after)
- Check-in time per patient
- Visit start time accuracy
Quality Metrics
- Data accuracy (errors caught in review)
- Insurance verification success rate
- Missing information incidents
Experience Metrics
- Patient satisfaction with intake process
- Staff satisfaction
- Provider feedback on information quality
Getting Started
A practical implementation path:
Phase 1: Foundation (Weeks 1-4)
- Evaluate current intake process
- Document time spent, pain points
- Research solutions
- Define requirements
Phase 2: Selection (Weeks 5-8)
- Evaluate vendors
- Demo solutions
- Check references
- Make selection
Phase 3: Implementation (Weeks 9-16)
- Configure system
- Build/customize forms
- Integrate with EHR
- Train staff
Phase 4: Pilot (Weeks 17-20)
- Launch with subset of appointments
- Monitor closely
- Gather feedback
- Iterate based on learnings
Phase 5: Full Launch (Week 21+)
- Roll out to all appointments
- Continue monitoring
- Optimize based on data
The Bottom Line
AI-powered intake isn’t just about eliminating clipboards—it’s about reclaiming hours of staff time, improving data accuracy, and creating better experiences for patients and staff alike.
The technology is mature and proven. The question isn’t whether digital intake works, but which solution fits your practice and how to implement it effectively.
Ready to Modernize Your Intake Process?
We help medical practices implement AI-powered intake solutions that integrate with existing systems and workflows.
Contact us to discuss intake automation →
Or call us directly: (678) 824-2420